Do you trust your memory for a lot of things? Do you ever forget if something happened a week ago or two weeks ago? Do you ever complete a routine task without concentrating on it and later wonder if you did it? I have been in all these places at one time or another. Sometimes the person I’m caring for can help me out. Other times my person has been too young, too sick, struggling with dementia, or maybe just as distracted as I am. Learning to keep records would save me in these situations, and I admit I haven’t got this down perfectly. But, there are a few things I’ve found helpful.
I have started the habit of writing things down, and keep paper and pencil in multiple places. Even the things I think I’m going to remember may get clouded with other facts and happenings. My aunt and uncle keep a calendar close to their phone and write down their appointments when they get a reminder call. I use a datebook for appointments but also to record significant events, like a fall, the start of a new symptom or a medication side effect. Doctors often ask about these things so the datebook always goes along to appointments.
Another good use for your notebook is to record blood pressure readings if your “person” has hypertension and is on medication for that. Ideally, the doctor will want to have BP taken each day, at the same time of day and with the same monitor, until he knows the medication is working well. If you are buying a blood pressure monitor, get one that records date, time and pressure and stores the information for later reference.

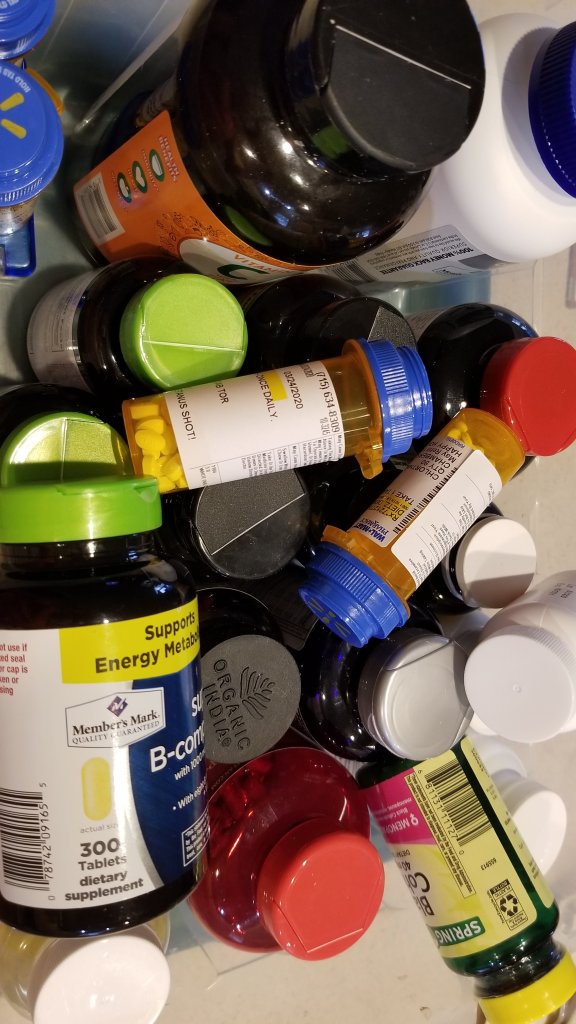
Monitoring medications is one of the more serious tasks of caregiving, and it does require keeping records. A helpful website for this is Drugs.com. It keeps track of all the medications and their possible interactions for anyone who cares to make a free account and input their information. It’s almost like having your own personal pharmacist.
I love to make use of online apps that help me connect with doctors and clinics. Our rural clinic gives access to primary care and specialty docs through a health app that keeps track of all appointments, visit summaries, and medication lists. As a caretaker I had to set up my family members’ accounts and sign the necessary legal papers (proxies) to have access to their records. All four of the people I help through the app are linked to my own account and I only need one password. I can ask questions and get answers for them, change appointments when necessary, and see test results. This has been especially helpful during this pandemic time.

Don’t forget that if you have a smart phone, you have a valuable helper. I took pictures of all my husband’s supplements and medications, which can be referenced any time someone asks me about dosages. I also put my family members birth dates, addresses, and doctor’s names in the notes section of their contact record on my phone. It really helps to have that information handy when filling out forms at doctor’s offices.
And do you have a file cabinet? I do. I have folders for our medical, dental and vision visits and bills. I also have files for those papers from insurance companies that tell you what they’ve been billed. I’ve heard so much about insurance fraud and if I see procedures that I don’t recognize, I ask questions. I don’t always understand what I’m seeing, but I’m afraid to throw them away (most of the time.)
Start your stash of records now and keep them up to date.